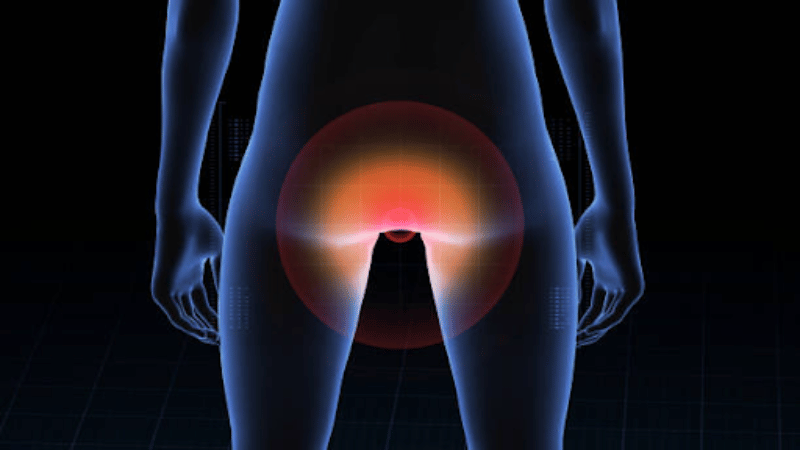
Hemorrhoids, those uncomfortable and often embarrassing lumps around your anus, are a common concern for many. But what happens when symptoms overlap with something more serious, like colorectal cancer? March is Colorectal Cancer Awareness Month, an important time to understand the differences and similarities between these two conditions. Some may attribute their symptoms to ‘just hemorrhoids’, potentially delaying a proper diagnosis until their symptoms become more severe.
With colorectal cancer affecting approximately one in 24 people and becoming increasingly prevalent in younger adults, it’s important to recognize the signs and when to seek medical advice.1
Hemorrhoids, which are swollen blood vessels in or around the anus, are not a sign of colorectal cancer (also known as colon cancer). However, symptoms of hemorrhoids, such as rectal bleeding, can indicate cancer when paired with other symptoms. This is where confusion often arises, and why it’s important to stay vigilant about your colorectal health. If your symptoms are related to internal hemorrhoids, USA Hemorrhoid Centers can help.
Learn When to Seek Medical Attention for Hemorrhoids

Understanding Hemorrhoid Symptoms
Hemorrhoids are uncomfortable swollen veins around the anus, and it’s estimated that about one in 10 people experience them. Hemorrhoids can affect people of any age, but they are most common in people between the ages of 45 and 65.
Hemorrhoids come into two forms: internal and external. External hemorrhoids are located around the anus and are more noticeable. They also tend to be more painful than internal hemorrhoids because of their location, which has more nerve endings.
No matter whether they are internal or external, hemorrhoids can cause a range of painful symptoms including:
- Bleeding
- Itching around the anus
- Mucus discharge
- Feelings of fullness after defecating
- Uncomfortable bowel movements
Hemorrhoid symptoms often improve within a few days to a week and are generally benign. It’s important to be aware, however, that internal hemorrhoids can take longer to heal and may get progressively worse. When internal hemorrhoids are left untreated, they can start to protrude out of the anus, a condition known as prolapse. Prolapsed hemorrhoids can cause significant pain and may need medical interventions to treat them, such as hemorrhoid artery embolization (HAE).
Learn About the Benefits of HAE

Colorectal Cancer: What You Need to Know
Colorectal cancer is a polyp that forms inside the colon or rectum. Most polyps are benign but have the potential to turn into cancer. Out of the 150 thousand people diagnosed with colon cancer each year, a third of them will not survive.
Colorectal cancer mainly affects adults over the age of 50, but genetics can also play a role in cancer risk. Your risk can also increase if you:
- Eat a diet high in red meat or low in fiber.
- Smoke or used to smoke.
- Are overweight or obese.
- Have inflammatory bowel disease (IBD).
Some of these risk factors, such as eating a low-fiber diet and having IBD, are also risk factors for hemorrhoids.
Early-stage colon cancer doesn’t usually present symptoms. However, some symptoms of colorectal cancer, such as rectal bleeding, can also overlap with hemorrhoid symptoms, including:
- Chronic abdominal pain, cramps, or gas
- Changes in bowel habits (diarrhea, constipation, very thin stools, or bloating)
- Incomplete bowel movements due to blockage
- Fatigue
- Unintentional weight loss
In this case, a gastroenterologist or oncologist may be the best option in finding care for colorectal cancer.

Hemorrhoids vs Cancer: How to Tell the Difference
Hemorrhoids and colorectal cancer can share similar symptoms, but these symptoms can present differently. The table below illustrates the difference.
| Symptoms | Hemorrhoids | Colorectal Cancer |
|---|---|---|
| Rectal Bleeding | Bright red blood, often painless | Dark red blood mixed with stool, persistent bleeding |
| Bowel Habit Changes | Temporary changes, often linked to diet | Persistent changes with unexplained constipation or diarrhea |
| Pain and Discomfort | In prolapsed hemorrhoids, pain localizes in the anus, often while sitting down | Polyps can cause abdominal or back pain |
Even if you experience most of these symptoms, it’s important not to self-diagnose. Gastrointestinal conditions like irritable bowel disease (IBD), irritable bowel syndrome (IBS), Crohn’s disease, and ulcerative colitis can have similar symptoms.
A hemorrhoid specialist may be able to determine what’s causing your symptoms and recommend the best course of action. USA Hemorrhoid Centers can discuss non-surgical treatment options if your symptoms are synonymous with hemorrhoids.
Get an Expert Opinion By Scheduling Online

Why Colorectal Cancer Screenings Matter
Early detection and treatment of colorectal cancer significantly improve survival rates, with stage I at a 91 percent survival rate compared to only 15 percent for stage IV. It’s recommended to start colon cancer screenings after 45, and younger if you have a family history. Some diagnostic tests to identify hemorrhoids, such as colonoscopy, can be used to detect colorectal cancer.
When Hemorrhoid Treatment is Required
Some hemorrhoids are not able to go away after a week despite using natural remedies. If you are experiencing hemorrhoid symptoms for more than a week, you may need medical treatment. Additionally, you should seek help from a hemorrhoid specialist if you have:
- Persistent or severe bleeding
- Worsening pain and swelling
- Internal hemorrhoid bulging outside the anus (prolapsed hemorrhoid)
If a hemorrhoid is left intreated, you increase your risk of blood clots in the affected area, known as thrombosed hemorrhoids. You are also at an increased risk of developing anemia, anal fissures, or an infection. The earlier hemorrhoids are treated, the risk of complications decreases.
Treatment at USA Hemorrhoid Centers
If your symptoms are caused by hemorrhoids, USA Hemorrhoid Centers specializes in treating hemorrhoids with hemorrhoid artery embolization (HAE).
HAE is an innovative, minimally-invasive procedure that’s designed to reduce blood flow to the hemorrhoid and alleviate symptoms for lasting relief. No incisions are made, and the procedure doesn’t come with a week-long, residual pain like rubber band ligation does.
If your symptoms are more consistent with hemorrhoids, such as painless rectal bleeding, itching, or mucus discharge, contact us by calling or scheduling an appointment online.
Frequently Asked Questions
Can hemorrhoids cause cancer?
Hemorrhoids do not cause cancer, but symptoms of colorectal cancer can sometimes overlap with hemorrhoids and can happen simultaneously.
Do hemorrhoids increase colorectal cancer risk?
Hemorrhoids do not increase colorectal cancer risk, but both conditions share similar risk factors such as diet, age, smoking status, and inflammatory bowel disease (IBD).
Can colorectal cancer be mistaken for hemorrhoids?
Colorectal cancer can be misdiagnosed as hemorrhoids, especially in younger people. This can lead to delayed treatment and increase mortality risk.
What are the top two signs of colorectal cancer?
Major indicators of colorectal cancer include persistent diarrhea or constipation in addition to dark, red blood in the stool.